For decades, surgery has been a discipline of “averages”—surgeons applied techniques that worked for the average patient, adjusted by their own intuition and experience. But as we move through 2026, the arrival of the Human Digital Twin (HDT) has ushered in the era of “One-Size-Fits-One” medicine. This is no longer just about viewing a 3D scan on a monitor; it is about creating a living, breathing virtual replica of a patient that mirrors their unique anatomy, physiological responses, and even their long-term healing patterns.
Defining the Surgical Digital Twin (SDT)
In 2026, the medical community distinguishes between simple 3D reconstructions and the Shadow Twin. While a standard model might show the shape of a heart, a Shadow Twin integrates real-time data to simulate biomechanical properties like tissue elasticity and fluid dynamics.
By fusing MRI/CT scans with genomic data and real-time inputs from clinical-grade wearables, the HDT becomes a functional simulation. It doesn’t just look like the patient; it behaves like them. If the patient has high blood pressure or brittle bones due to a specific genetic marker, the twin reflects those exact constraints during a virtual rehearsal.
Building the Twin: Data Fusion and Multimodal AI
Creating a high-fidelity twin requires a massive synthesis of disparate data points. This process, often called “Twinning,” is powered by Multimodal AI architectures that can ingest and harmonize:
- Structural Data: High-resolution imaging (CT, MRI, Ultrasound).
- Biological Data: Proteomics, metabolomics, and the patient’s unique genetic code.
- Real-time Telemetry: Heart rate variability, oxygenation, and glucose levels from IoT-connected devices.
Stages of Digital Twin Maturity in 2026
| Maturity Level | Type | Capabilities | Clinical Value |
| Level 1 | Digital Model | Static 3D reconstruction from scans. | Visual reference only. |
| Level 2 | Digital Shadow | One-way data flow (scans + history). | Static preoperative planning. |
| Level 3 | Functional Twin | Two-way data; simulates physiology. | Risk-free rehearsal; haptic testing. |
| Level 4 | Intelligent Twin | Predictive AI; simulates long-term outcomes. | GPS for surgery; outcome forecasting. |
Preoperative Simulation: The Risk-Free Testbed
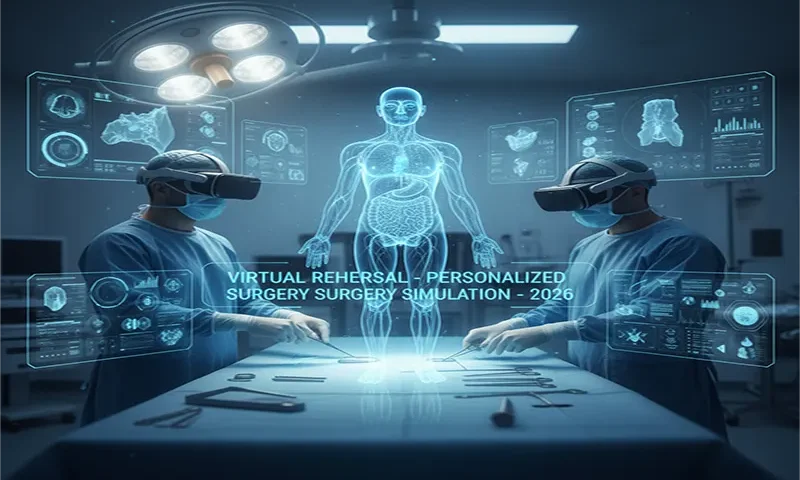
The most immediate impact of HDTs is the “Virtual Dry Run.” Before the first incision is made in the physical world, a surgeon can perform the entire operation in a high-fidelity VR environment.
Haptic Physics and Finite Element Analysis (FEA)
Using Finite Element Analysis (FEA), the simulation calculates the physics of every move. When a surgeon “cuts” virtual tissue, the haptic feedback controllers provide the exact resistance of that specific patient’s tissue. In orthopedic surgery, FEA allows doctors to see the stress distribution on a bone after an implant is placed, identifying potential fracture points years before they occur.
Structural Heart and Skull Base Cases
Institutions like Johns Hopkins and Duke University have become leaders in using digital twins for structural heart valve replacements. By simulating the blood flow (hemodynamics) through a virtual valve, surgeons can select the perfect size and placement to prevent post-operative leaks, reducing emergency complications by up to 25%.
Intraoperative “Shadowing” and Spatial Computing
The utility of the twin does not end when the surgery begins. In 2026, the digital twin is projected onto the patient in the operating room via Holographic Augmented Reality (AR).
This creates a “GPS for the body.” As the surgeon operates, the twin updates in real-time to account for tissue shifts or bleeding—a process known as Intraoperative Shadowing. Using spatial computing headsets, the surgeon can “see through” skin and bone to locate hidden vessels or the exact boundaries of a tumor that might have shifted since the last scan. This level of precision has reduced average operative times by up to 20% at leading medical centers.
The Future of Outcome Prediction
Beyond the operating room, the HDT is a time machine. By accelerating the simulation, doctors can see how a patient will heal over the next six months or how a prosthetic joint will wear over the next decade. This predictive power allows for Personalized Recovery Protocols, where physical therapy and medication are tailored to how the virtual twin responded to the simulated surgery.
Challenges and Bioethics: Who Owns Your Virtual Self?
The rise of HDTs has sparked a fierce debate over Digital Ownership. In 2026, the “Digital Self” is considered an extension of the physical person.
- Data Dominion: Current ethical frameworks emphasize that individuals, not hospitals or AI vendors, should be the primary stewards of their digital twins.
- The Trust Gap: To ensure safety, all surgical twins must undergo Verification, Validation, and Uncertainty Quantification (VVUQ) to prove that the virtual simulation accurately represents the physical reality.
From Reactive to Predictive
The human digital twin has moved surgery from a reactive discipline to a predictive science. We no longer wait for a complication to happen to know it was a risk; we discover it in the virtual world first. By 2026, the “virtual rehearsal” has become a standard of care for complex cases, ensuring that when the surgeon finally picks up the scalpel, they have already performed the successful operation a dozen times.